Burns Trauma:严重热损伤中的肝素抵抗:一项前瞻性队列研究
2021-11-01 MedSci原创 MedSci原创
低分子量肝素(LMWH)常规用于烧伤患者以预防血栓形成。临床上将定义为AFXa活性<0.2 IU/ml定义为肝素抵抗,这一现象在严重烧伤患者中非常普遍 (>70%)。一些研究报告了肝素耐药
低分子量肝素(LMWH)常规用于烧伤患者以预防血栓形成。临床上将定义为AFXa活性<0.2 IU/ml定义为肝素抵抗,这一现象在严重烧伤患者中非常普遍 (>70%)。一些研究报告了肝素耐药性,但尚未系统地研究其机制和患病率。
这是第一项测量重度烧伤肝素抵抗的系统前瞻性研究,并检验了来自 NET 和其他来源的核糖体可能会损害肝素抗凝能力的假设。
图1 文章来源
研究人员假设,由组蛋白结构组成的核糖体与相关的DNA从受伤的组织和激活的免疫细胞中以中性粒细胞外陷阱(NETs或NETosis)的形式释放出来,可以中和 LMWH,导致抗凝效果不佳,并计划通过抗 Xa 因子活性的降低来评估。
在接受LMWH治疗的第5、10和14天, 从>15%全身表面积(TBSA)烧伤患者取血。测量峰值抗因子Xa(AFXa)活性、抗凝血酶(ATIII)活性、无细胞DNA(cfDNA)水平和核糖体水平。混合效应回归对多个混杂因素进行了调整,其中包括损伤严重程度和 ATIII 活性,并用于测试核小体和 AFXa 之间的关联。
该研究共纳入 30 名严重烧伤患者,平均TBSA 43%(SD 17)。23名(77%)患者受到肝素抵抗的影响。
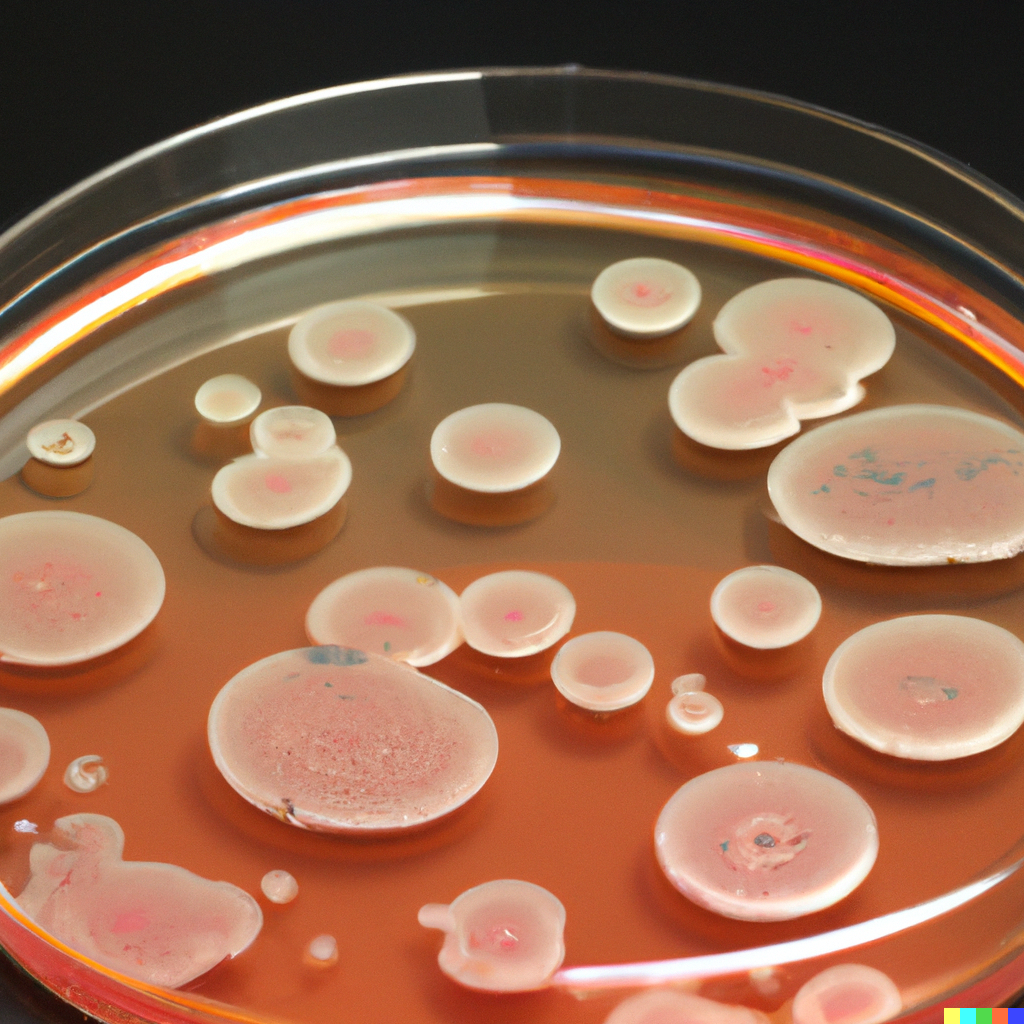
所有样本的平均AFXa活性峰值为0.18 IU/mL(SD 0.11)。平均ATIII的活性为81.9%(SD 20.4)。发现以较高 LWMH 剂量采集的样品具有显着增加的 AFXa 活性,尽管在所有剂量下均未观察到该效果,但在 8000 IU 时,没有样品对肝素具有抗性。核糖体水平与AFXa呈负相关(r = -0.29, p = 0.050),与假设一致。
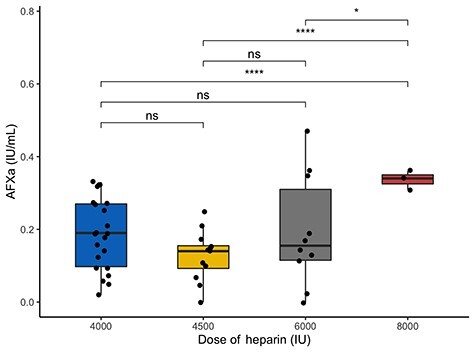
图2峰值抗 Xa 因子 (AFXa) 水平随着 LMWH 剂量的增加而增加。
最终模型以AFXa峰值为响应变量,对核糖体水平(p = 0.0453)、ATIII活性(p = 0.0053)、样本前LMWH剂量(p = 0.0049)、给药(依诺肝素或丁扎肝素)(p = 0.03)和其他混杂因素包括损伤的严重程度、年龄、性别、样本的时间点进行调整。
肝素抵抗是严重烧伤的普遍问题。烧伤后核糖体水平升高,并显示与峰值抗因子 Xa 水平(低分子量肝素抗凝能力的衡量指标)降低有关。这与它们可能干扰体内肝素的抗凝作用并导致肝素抵抗的假设一致。
据此,研究人员建议在严重烧伤后调整剂量时准确监测AFXa的活性,并制定适当的治疗升级计划。
原始文章
Cato Liam D,Bailiff Benjamin,Price Joshua et al. Heparin resistance in severe thermal injury: A prospective cohort study.[J] .Burns Trauma, 2021, 9: tkab032.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#前瞻性队列#
116 举报
#前瞻性#
103 举报
#前瞻性队列研究#
116 举报
#TRA#
122 举报
#Trauma#
129 举报
#损伤#
108 举报
不断学习不断进步
132 举报