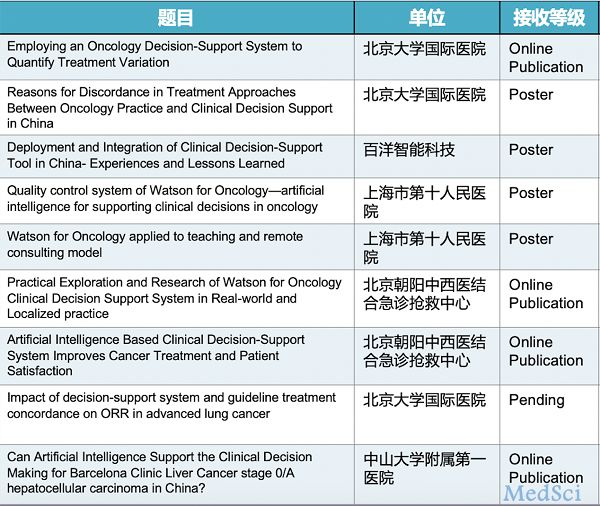
卡妥索单抗治疗晚期胃癌伴腹膜转移临床研究成果入选2022ASCO年会
2022-05-30 网络 网络
凌腾医药是一家专注于T细胞衔接抗体开发的临床阶段生物制药公司。该公司今日宣布,美国临床肿瘤学会(American Society of Clinical Oncology, ASCO)已接收卡妥索单抗
凌腾医药是一家专注于T细胞衔接抗体开发的临床阶段生物制药公司。该公司今日宣布,美国临床肿瘤学会(American Society of Clinical Oncology, ASCO)已接收卡妥索单抗治疗晚期胃癌伴腹膜转移的Ⅲ期临床试验第一阶段研究成果作为摘要发布。
此次公布了卡妥索单抗治疗晚期胃癌伴腹膜转移国际多中心Ⅲ期临床试验第一阶段(Stage 1)cohort A的临床数据(clinicaltrials.gov: NCT04222114)。全球每年胃癌新发病例超过100万例【1】,50%以上的晚期胃癌患者在根治性切除术后出现腹膜转移,且部分合并有恶性腹水,严重影响生活质量【2】。由于目前缺乏对晚期胃癌伴腹膜转移的针对性疗法,这类患者在三线全身治疗失败后的预期生存期仅为2.3-2.4个月。cohort A入组的9名患者(1/3的患者已接受三线治疗)接受卡妥索单抗治疗后,中位总生存期(median overall survival)为3.4个月,伴有较明显的腹水消退。卡妥索单抗已初步展现在该适应症上的治疗潜力。
Reference
1. World Health Organization (WHO). Globocan 2020. Global Cancer Observatory. Accessed January 7, 2021. https://gco.iarc.fr/
2. 季加孚,沈琳,徐惠绵,徐瑞华,朱正纲,程向东,刘云鹏,李子禹,陕飞,孙宇,唐磊,周军,张小田.胃癌腹膜转移防治中国专家共识[J].中华胃肠外科杂志,2017,20(05):481-490.
关于卡妥索单抗
卡妥索单抗于2009年获得了欧洲药品管理局批准用于治疗EpCAM阳性恶性肿瘤引起的恶性腹水,是全球第一个上市的T细胞衔接双特异性抗体药物。卡妥索单抗结合肿瘤相关性抗原EpCAM和T细胞的CD3受体,同时通过与FcɣR招募免疫附属细胞,协同T细胞杀伤肿瘤细胞并产生潜在的肿瘤疫苗作用。目前,卡妥索单抗胃癌适应症正开展国际多中心Ⅲ期临床试验(NCT04222114),膀胱癌适应症正开展Ⅰ/Ⅱ期临床试验(NCT04799847)。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#临床研究成果#
164 举报
#研究成果#
0 举报
#ASC#
87 举报
#晚期胃癌#
149 举报
#腹膜转移#
101 举报
#腹膜#
134 举报