Complement Ther Med:VR项目可作为围手术期疼痛控制的辅助工具
2020-09-26 网络 网络
手术后的疼痛控制和麻醉药的过度使用对所有领域的外科医生来说都是具有挑战性的问题。虽然虚拟现实(VR)已经越来越多地应用于各个领域,但其在围手术期的可行性和有效性尚未得到评估。本研究旨在检查围手术期环境
手术后的疼痛控制和麻醉药的过度使用对所有领域的外科医生来说都是具有挑战性的问题。虽然虚拟现实(VR)已经越来越多地应用于各个领域,但其在围手术期的可行性和有效性尚未得到评估。本研究旨在检查围手术期环境中集成VR协议的经验,研究结果已在线发表于Complement Ther Med。

将在一家机构接受微创前路手术的患者随机分配接受一系列的VR冥想/心态治疗(VR)或术后标准护理(非VR)。追踪患者术后疼痛水平、麻醉剂使用情况和满意度。
结果,纳入52名患者,每组26人。两组患者术后疼痛评分、麻醉剂总利用率和总体满意度评分无显著差异。对于VR臂的患者,疗程能够纳入围手术期常规,几乎不受干扰。大多数人(73.9%)能够完成全部6个VR疗程,并表示在使用该设备时疼痛、焦虑和恶心评分较低。很大一部分人表示他们会再次使用VR(76.2%)或希望有一个针对疼痛的VR程序(62.0%)。没有出现设备使用相关的并发症。
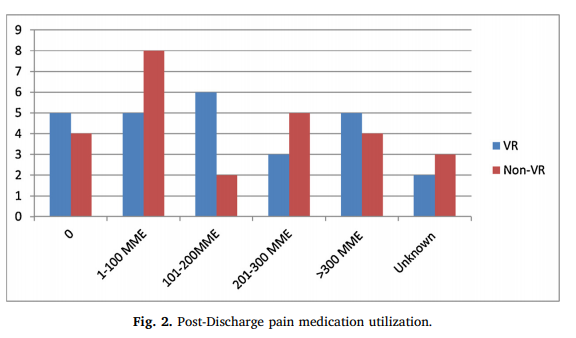
综上所述,该研究结果表明,VR是一种安全和简单的干预措施,与患者的高满意度相关,并可在围手术期环境中实施。虽然目前的研究不足以检测到麻醉剂使用的差异,但该设备有望成为围手术期多模式疼痛和焦虑控制的辅助工具。
原始出处:
Kelly R Haisley, Olivia J Straw, et al., Feasibility of implementing a virtual reality program as an adjuvant tool for peri-operative pain control; Results of a randomized controlled trial in minimally invasive foregut surgery. Complement Ther Med. 2020 Mar;49:102356. doi: 10.1016/j.ctim.2020.102356. Epub 2020 Feb 26.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#手术期#
68 举报
#MPL#
80 举报
#Complement#
104 举报
#Med#
69 举报