J Virol:盐霉素可通过干扰核内体的酸化和病毒基质蛋白2的功能抑制流感病毒感染
2019-01-02 Etrgh 病毒学界
流感病毒是造成人和动物呼吸道感染的重要病原,该病毒传染性强,且容易发生变异导致感染人或动物的高死亡率。金刚烷胺、奥司他韦及扎那米韦是目前较为常用并能有效抑制流感病毒的药物,但由于流感病毒毒株容易发生变异,造成这些药物的有效性在不断减弱。
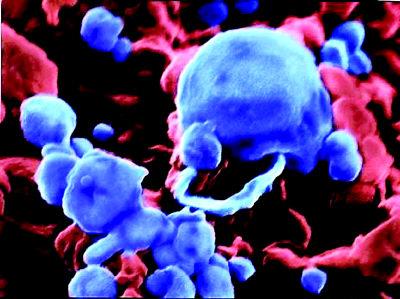
流感病毒是造成人和动物呼吸道感染的重要病原,该病毒传染性强,且容易发生变异导致感染人或动物的高死亡率。金刚烷胺、奥司他韦及扎那米韦是目前较为常用并能有效抑制流感病毒的药物,但由于流感病毒毒株容易发生变异,造成这些药物的有效性在不断减弱。开发和筛选更加有效的抗病毒药物迫在眉睫。近日,来自韩国的科学家通过筛选,在2000种合成化合物中,发现了一种能够有效抑制流感病毒感染的化合物-盐霉素。该研究成果目前已发表至《Journal of Virology》杂志,题为“Salinomycin Inhibits Influenza Virus Infection by Disrupting Endosomal Acidification and Viral Matrix Protein 2 Function”。
科学家通过进一步深入研究发现,盐霉素是直接通过阻断病毒基质蛋白质子通道的活性来抑制流感病毒的感染。更值得注意的是,在小鼠试验中发现,同时口服盐霉素和奥司他韦具有联合增强抗病毒的效果。
该研究研制出了新的抗病毒合成药物-盐霉素,并且通过小鼠试验发现盐霉素和奥司他韦联合使用能有效提高抗病毒的效果,进一步开发用于临床抗病毒治疗新药物奠定了基础。
原始出处:Jang Y, Shin JS, Yoon YS, et al. Salinomycin Inhibits Influenza Virus Infection by Disrupting Endosomal Acidification and Viral Matrix Protein 2 Function. J Virol. 2018 Nov 27;92(24).
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Virol#
88 举报
#基质#
86 举报
学习了
112 举报