皮肤伤口基质的效用与局部组织重排和游离皮瓣重建对肿瘤性头皮伤口的比较
2022-02-16 MedSci原创 MedSci原创
局部组织重排、游离皮瓣重建和双层伤口基质代表了覆盖头皮缺损的重建方式;然而,仍不明确何种作为首选方法更加合适。
局部组织重排、游离皮瓣重建和双层伤口基质代表了覆盖头皮缺损的重建方式;然而,首选指示不太清楚。
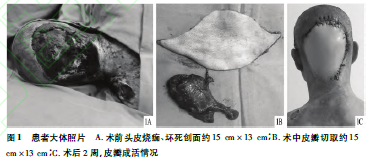
图1文章来源
研究者旨在评估这些干预措施的有效性,故回顾性分析(2008年至2019年)需要软组织重建肿瘤头皮伤口的受试者,并据此比较了90天的伤口覆盖率、住院时间、手术时间和伤口并发症。受试者被双重匹配成两个对照组:(1)局部组织重排与双层伤口基质,(2)游离皮瓣重建与双层伤口基质。
结果显示,该研究共纳入361名受试者。匹配后,126名受试者组成局部组织重排与双层伤口基质队列,56名受试者组成游离皮瓣重建与双层伤口基质队列。
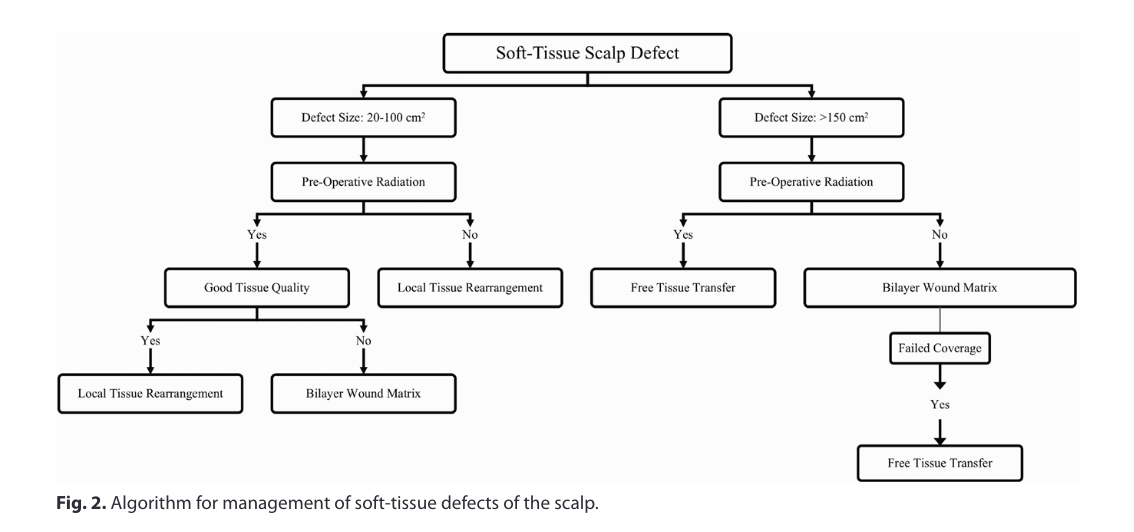
图2头皮软组织缺损处理算法
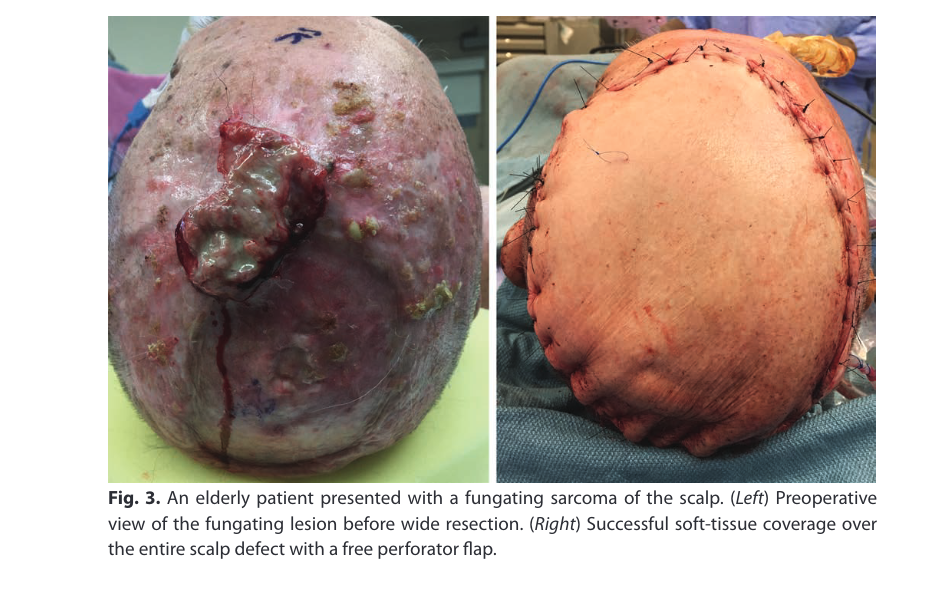
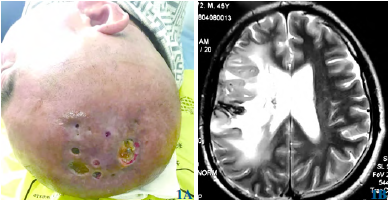
图3。一位老年患者表现为头皮真菌肉瘤。(左)广泛切除前真菌病变的术前视图。(右)用游离穿支皮瓣成功覆盖整个头皮缺损。
局部组织重排/双层伤口基质中值缺损大小为35±42.5 cm2。与双层伤口基质(84.1%)相比,局部组织重排在90天时提供了显著更好的伤口覆盖年龄(95.2%)(p<0.040)。
游离皮瓣重建/双层伤口基质队列中的中值缺损大小为100±101.1 cm2。
90天的成功率(游离皮瓣重建,92.9%;双层伤口基质,96.4%;p<1.00)和再次手术率(14.3%vs3.6%;p<0.352)相似。然而,游离皮瓣重建的手术时间显著延长(418分钟,vs100分钟;p<0.001)。
局部组织重排、游离皮瓣重建和双层伤口基质都是头皮重建的首选方法。对于较小的伤口(<100 cm2),局部组织重排可能比双层伤口基质更可靠。对于较大的缺损(150至250 cm2),双层伤口基质可能具有与游离皮瓣重建相当的疗效,并且考虑到与游离皮瓣重建相关的更长的手术时间和住院时间,可能更具成本效益。
原始文章:
Othman, Sammy, Shakir, Sameer, Azoury, Said, et al. Utility of Dermal Wound Matrices Compared with Local-Tissue Rearrangement and Free Flap Reconstruction for Oncologic Scalp Wounds: A Multidisciplinary Dual Matched-Pair Analysis. Plast Reconstr Surg. 2022;149(2):469-480. doi:10.1097/PRS.0000000000008774.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#基质#
123 举报
#局部#
95 举报
#皮瓣#
107 举报