硫胺素、维生素 C 和氢化可的松联合治疗脓毒症和感染性休克
2022-03-01 MedSci原创 MedSci原创
最近的一项研究表明,2017年全球估计有1100万例败血症相关死亡,占总死亡人数的19.7%。在脓毒症患者中经常检测到维生素C和硫胺素的缺乏,据报道,这归因于摄入量减少和代谢需求增加。
最近的一项研究表明,2017年全球估计有1100万例败血症相关死亡,占总死亡人数的19.7%。在脓毒症患者中经常检测到维生素C和硫胺素的缺乏,据报道,这归因于摄入量减少和代谢需求增加。
 图1文章来源
图1文章来源
该研究评估硫胺素和维生素C联合或不联合氢化可的松治疗脓毒症和感染性休克的临床疗效,共涉及8项RCT,共1428名患者。
结果显示,与安慰剂组相比,接受维生素C和硫胺素联合或不联合氢化可的松治疗的败血症和感染性休克患者的短期死亡率没有显着降低{风险比(RR),1.02[95%置信区间(CI)),0.87至1.20], p =0.81, I 2 =0%; 风险差(RD),0[95%CI,-0.04至0.05]}。
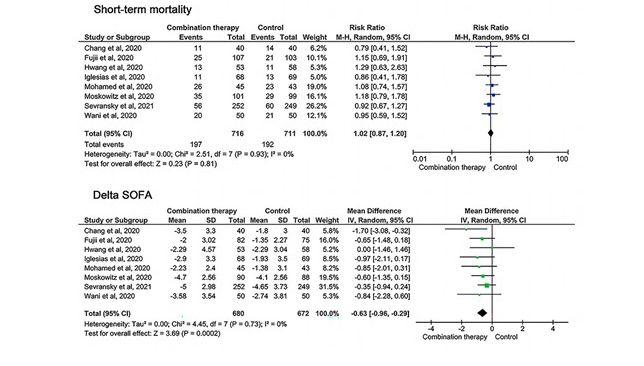
图2脓毒症患者短期死亡率和 delta SOFA 的森林图,比较了维生素 C 和硫胺素联合或不联合氢化可的松与安慰剂的联合治疗。
然而,联合治疗与SOFA评分[平均差(MD),-0.63,(95%CI,-0.96to-0.29, p <0.001, I 2 =0%]和血管加压药持续时间(MD,-22.11[95%CI,-30.46至-13.77],p <0.001,I2 =6%)。

图3短期死亡率和 delta SOFA 的试验序贯分析比较了败血症患者中维生素 C 和硫胺素加或不加氢化可的松与安慰剂的联合治疗。蓝色z曲线是通过应用随机效应模型绘制的。SOFA序贯器官衰竭评估
此外,其他结果的汇总估计值没有统计学差异。
研究显示,与安慰剂相比,维生素C和硫胺素联合治疗(加或不加氢化可的松)对短期死亡率没有影响,但与脓毒症和感染性休克患者的SOFA评分显着降低有关。
原始文章:
Renqi Yao, Yibing Zhu, Yue Yu, Zhixuan Li, Lixue Wang, Liyu Zheng, Jingyan Li, Huibin Huang, Guosheng Wu, Feng Zhu, Zhaofan Xia, Chao Ren, Yongming Yao, Combination therapy of thiamine, vitamin C and hydrocortisone in treating patients with sepsis and septic shock: a meta-analysis and trial sequential analysis,Burns & Trauma, Volume 9, 2021, tkab040
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#感染性#
117 举报
#学习#nice
158 举报
学习了
151 举报
#联合治疗#
126 举报
#氢化可的松#
136 举报
#硫胺素#
0 举报