Cell:科学家揭示小分子药物如何打开癌细胞中的“关闭按钮”!
2020-04-22 生物探索 生物探索
小分子DT-061可以特异性地稳定B56α-PP2A全酶,从而使其去磷酸化以达到抑癌效果。
已有研究表明,某些分子能够增加癌细胞中肿瘤抑制蛋白PP2A的活性,从而杀死癌细胞以缩小细胞系和动物模型中的肿瘤。但其作用机制尚不清楚。基于此,密歇根大学的科学家们发现小分子DT-061可以特异性地稳定B56α-PP2A全酶,从而使其去磷酸化以达到抑癌效果。该研究成果发表在《cell》期刊上。
 doi.org/10.1016/j.cell.2020.03.038
doi.org/10.1016/j.cell.2020.03.038
PP2A酶家族由三聚磷酸酶组成,即支架“A”亚基、催化“C”亚基和调节“B”亚基。其中,该蛋白的去磷酸化能力主要是由40多个决定特异性的调节“B”亚基竞争异质PP2A三聚体的组装和激活而调控的。通常一系列小分子PP2A激活剂(small molecule activators of PP2A,SMAPs)在一些体内肿瘤模型中可驱动c-Myc和ERK等特定致病底物的去磷酸化,从而协同抑制肿瘤。
小分子DT-061属于典型的SMAP,研究者利用细胞分离荧光素酶系统、免疫共沉淀(coIP)实验等,发现DT-061在细胞培养和体内都可以选择性地增强含有PP2A全酶种群的B56α。单独表达和纯化PP2A各亚基,发现DT-061可以直接稳定AB56αC异种三聚体。
 DT-061直接稳定AB56αC异种三聚体
DT-061直接稳定AB56αC异种三聚体
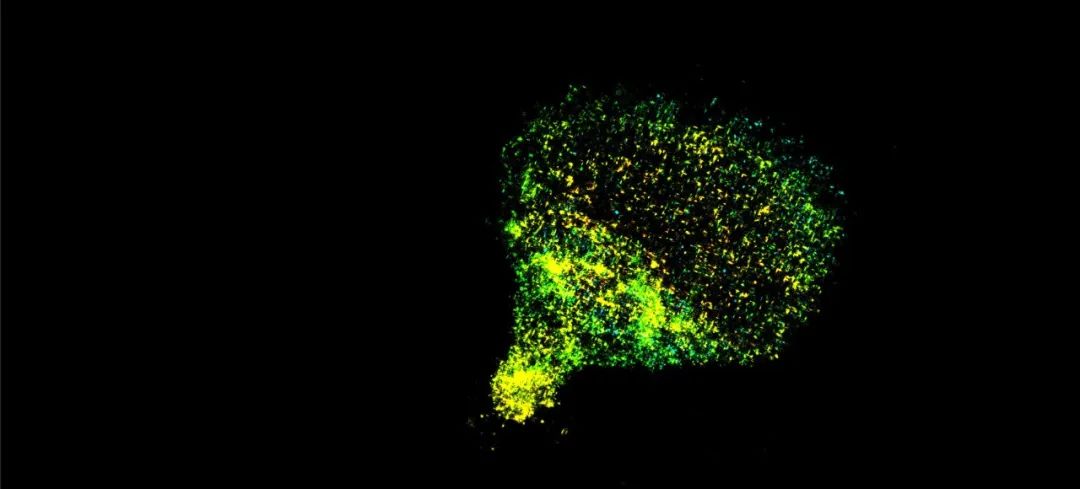
然后利用单粒子低温电子显微镜(cryo-EM)来观察药物结合PP2A复合体的三维结构,发现DT-061结合在PP2A亚基间的独特“口袋”中,并与所有三个PP2A亚基的残基相互作用,其独特的稳定机制帮助我们揭示了一个难以捉摸和不对称的磷酸酶异质三聚体的结构.
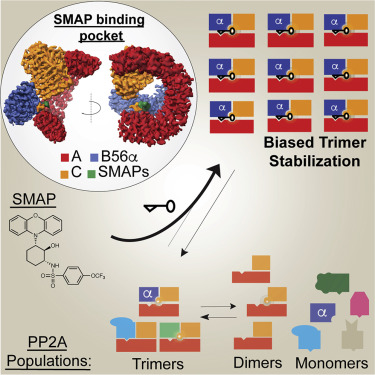 SMAPs选择性地稳定三亚单元以偏置磷酸酶PP2A
SMAPs选择性地稳定三亚单元以偏置磷酸酶PP2A
总之,研究者发现SMAPs结合在所有3个PP2A亚基间的“口袋”中,DT-061(SMAP)可以特异性稳定B56α-PP2A全酶,使后者可选择性地对底物如c-Myc去磷酸化。而甲基化的B56α异三聚体的积累可作为一种潜在的临床生物标志物。
研究者还表示,除了癌症,PP2A在心血管和神经退行性疾病等其他疾病中也出现失调现象,因此,该发现也为开发治疗心力衰竭和老年痴呆症等的新药提供了机会。
原始出处:
Daniel Leonard, Wei Huang, Sudeh Izadmehr, et.al. Selective PP2A Enhancement through Biased Heterotrimer Stabilization. Cell April 20, 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#CEL#
98 举报
#小分子#
82 举报
#Cell#
139 举报
#癌细胞#
95 举报